A healthcare conference will take place shortly to discuss an aspiration to achieve zero suicide (1). Of course no one would deny that this is a worthy aim. The programme reminds us that:
The Prime Minister has announced £2 million in funding for the Zero Suicide Alliance (ZSA) over the next 2 years. The funding will help to reduce suicides across the NHS, with the aim of achieving zero inpatient suicides.
If a person with suicidal tendencies has been admitted to a mental health facility, wouldn’t we expect them to be protected from themselves? Close observation and the prevention of access to a means for carrying out suicide would surely be expected as a matter of course. That is why they have been admitted. Similarly, when someone is admitted for an appendectomy, we would expect the availability of a surgeon to carry it out. It is true that some suicidal people are extremely clever and determined. Although zero inpatient suicide is the expected target, there may be an occasional person who manage to achieve it despite the best of measures. A fund of two million spread across numerous mental health facilities might be a help but it is hardly a bonanza. Also, it does not address suicide outside mental health facilities.
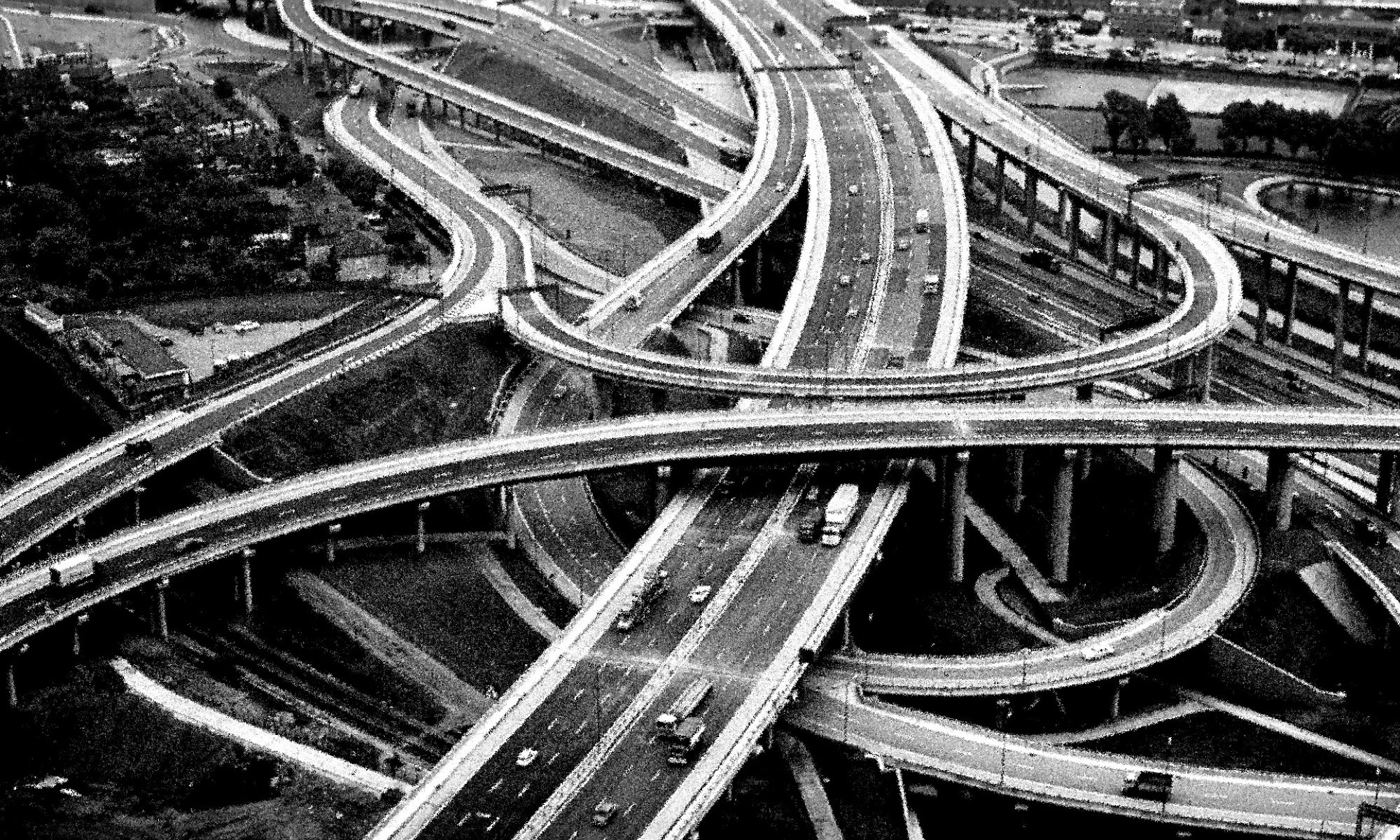
As regards the prevention of suicide across the population as a whole (including people in prison), the logistics of prevention are far from obvious. According to the Samaritans: just under 6,000 people take their own lives every year. [This compares with just under 2000 killed in road traffic accidents and around 25,000 seriously injured in this way annually]. In order for suicide to be preventable, it must be predictable. The recommendations set out in the Government’s Five Year Forward View for Mental Health policy on suicide prevention and reduction makes: a commitment to reduce suicides by 10% nationally by 2020/21 (1). This 10% reduction certainly has greater chance of success than 100%. However, people must get the kind of help that they want. It has been reported that one quarter to one half of people who have already attempted suicide do not attend follow-up appointments (2). A major stumbling block to prevention is that in primary care, where most depressed mood with suicidal tendencies is diagnosed, approximately three quarters of suicide deaths are of individuals who are unknown to secondary care services (3). Of various interpretations for this figure, the following are credible (a) that people who are liable to kill themselves conceal this fact successfully from others (b) that they are not taken seriously when they draw attention to their state of mind (c) that they are taken seriously but an appropriate service is not available (or available quickly enough) (d) that the kind of help available is unwanted or ineffective. Perhaps greater priority should be given to researching these possibilities than to inpatient services that should, in any case, be preventing suicide as part of their regular functions.
(1) Health Care Conference: Towards zero suicide. (2018). https://www.healthcareconferencesuk.co.uk/event/1224
(2) Miret, M., Ayuso-Mateos, J. L., Sanchez-Moreno, J., Vieta, E. (2013). Depressive disorders and suicide: Epidemiology and risk factors, and burden. Neuroscience and Biobehavioral Reviews, 37, pp. 2372-2374.
(3) Hawton, K., Casanas, I., Comabella, C., Haw, C., Saunders, K. (2013) Risk factors for suicide in individuals with depression: A systematic review. Journal of Affective Disorders, 147, pp. 17-28.